What FQHCs Teach Us About Meeting People Where They Are
A recent statewide study in Massachusetts reveals a story that is bigger than visit counts or hospitalization rates. It points to something more basic: where people feel comfortable showing up.
For many individuals living with serious mental illness, the most consistent point of contact in the system isn’t a specialty clinic, it’s their primary care provider. And in a lot of communities, Federally Qualified Health Centers (FQHCs) play that role. These are familiar places. People come in for routine medical issues, pick up medications, ask questions, and get support without navigating a separate behavioral-health system. Behavioral health isn’t carved out; it’s part of everyday care.
The findings comparing FQHCs to other outpatient settings reflect what clinicians have been seeing for years. When behavioral health is integrated into primary care, people stay connected. They schedule follow-ups. They refill prescriptions. They come back before symptoms escalate. Hospitalizations drop because relationships form early and stay stable, long before a crisis shows up.
But the higher emergency-department use within the FQHC group is an important reminder. Engagement alone isn’t enough without coordinated crisis pathways. Even with strong outpatient care, people still reach points where they need more support. That’s where the broader system matters: mobile crisis teams, diversion programs, real-time coordination tools, and partnerships that give providers a clearer picture of what’s happening when someone is struggling.
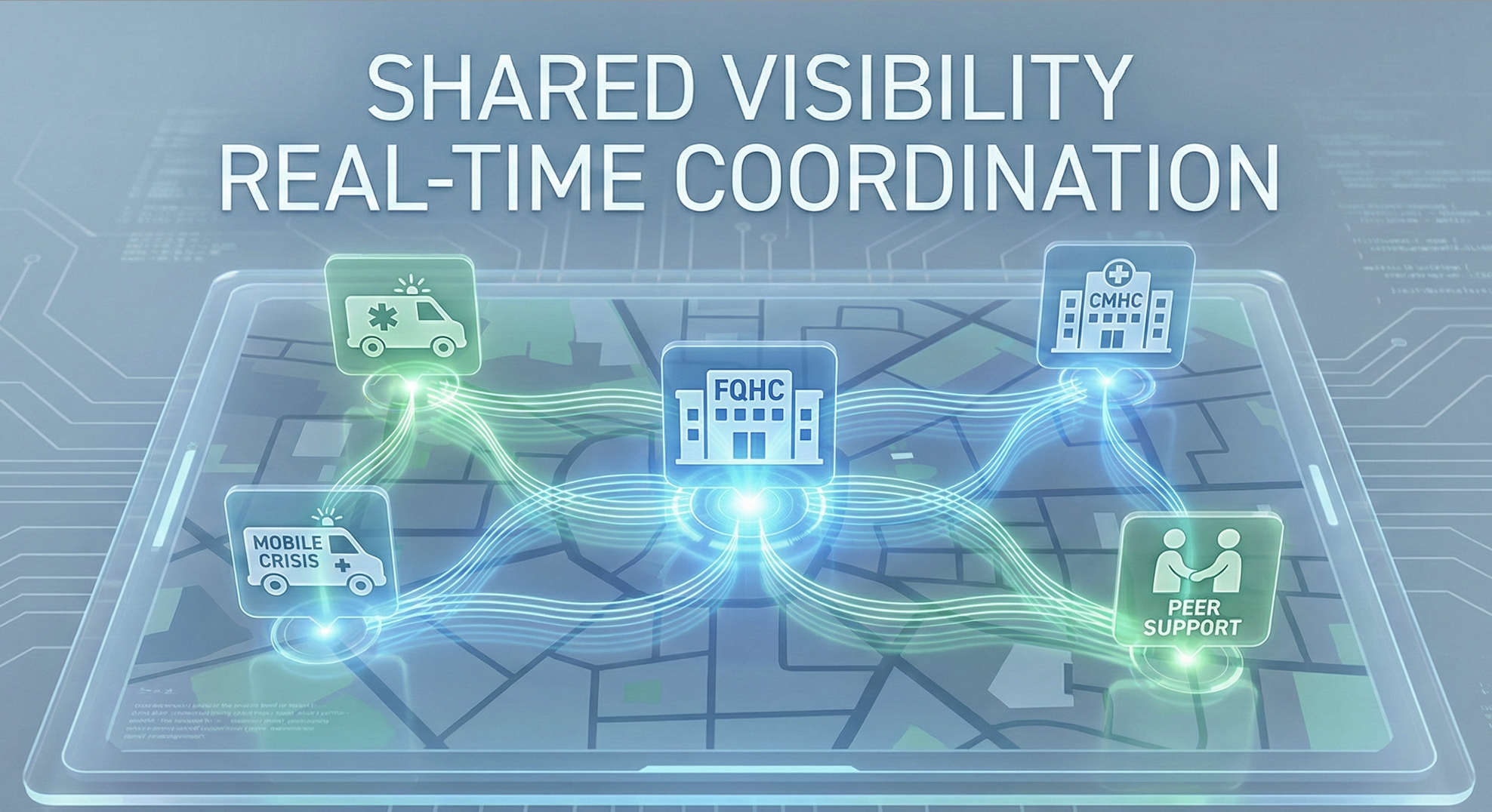
We see this play out every day. When an FQHC provider can quickly loop in a CMHC clinician, a crisis responder, a peer specialist, or a care manager—without losing time—the next step becomes easier for everyone involved. The person isn’t handed off into the void; they’re connected to a network that can actually follow through.
The study reinforces a truth that guides Cloud 9’s work: behavioral health starts wherever people already show up, not only in specialty settings. And when primary care and behavioral health move together in sync—supported by real-time communication and shared visibility, communities get stronger, crises reduce, and individuals find stability in places that already feel familiar.
The future isn’t just integrated care. It’s connected care, and every clinic, payer, and crisis team has a role to play in making that possible.






