Why Stability Matters in Mental Health
A new Australian study from Monash University has made a powerful case for rethinking how we address mental health, not just as a clinical concern, but as a systemic one. The researchers found that nearly one in three mental health conditions could be prevented through stronger social and economic policies - including financial security, safe housing, and cohesive communities.
This finding reinforces what many in behavioral health already know: treatment alone is not enough. Long-term wellbeing depends on community coordination, early support, and economic stability.
At Cloud 9, we believe that effective mental healthcare means aligning systems, not just offering services. Here’s what this study means for our customers and why integrated, community-based solutions are more critical than ever.
What the Research Shows:
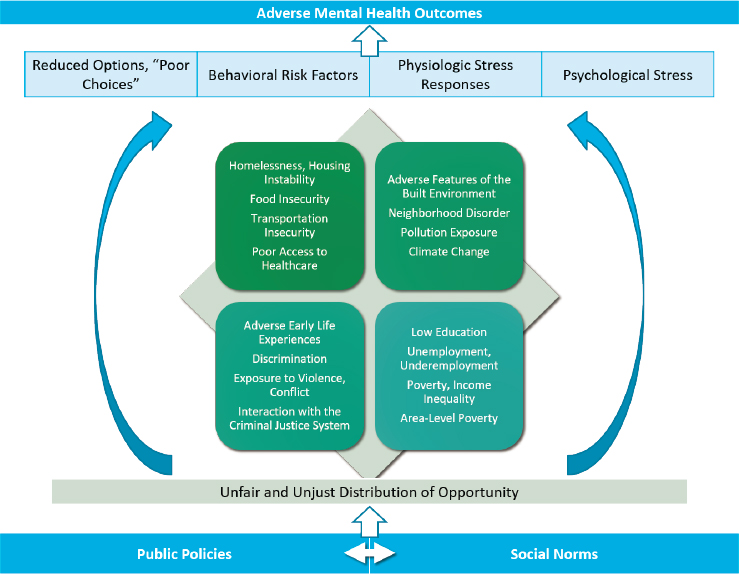
The Monash study analyzed the social determinants of mental health across multiple life stages. It found that people exposed to chronic insecurity, financial hardship, housing instability, or social isolation, were significantly more likely to develop mental health conditions later in life. In contrast, people who had access to basic protections like income stability, access to education, and trusted support systems experienced dramatically lower risk.
The key takeaway? Many behavioral health crises are preventable, but only if we treat root causes, not just symptoms.
Why This Matters for Cloud 9 Partners:
Community Mental Health Centers (CMHCs) & Certified Community Behavioral Health Clinics (CCBHC)s:
This research underscores the importance of wraparound care models. It’s no longer enough to offer therapy or medication alone - your teams are increasingly being asked to connect patients to housing, food access, and crisis support. Cloud 9 supports that model by coordinating between providers, social workers, and public agencies in real time. When CMHCs can respond as a system, outcomes improve and crises can be averted entirely.
Law Enforcement & First Responders:
First responders are often the first and sometimes the only point of contact for individuals in distress. But many of these calls stem from unmet social needs, not criminal behavior. This research validates what co-responder teams already practice: stabilization happens faster when we see the whole person. Cloud 9 helps frontline teams connect people to community-based services, ensuring that safety doesn't stop at the scene.
Managed Care Organizations (MCOs):
MCOs are increasingly being held accountable for outcomes that go beyond clinical care including housing stability, employment, and connection to services. Cloud 9 provides the data and interoperability that help MCOs track social drivers of health, coordinate with non-traditional providers, and reduce costly recidivism. Preventing a crisis costs far less than responding to one.
Federally Qualified Health Center (FQHCs) & Primary Care:
As the frontline for preventive care, FQHCs and primary care providers play a key role in identifying social risks early. But without the right tools, these risks stay unaddressed. Cloud 9 enables real-time alerts and care team collaboration, so behavioral health doesn’t fall through the cracks during routine checkups. Prevention doesn’t happen in isolation; it happens when systems connect.
Conclusion:
This research isn’t just a policy insight, it’s a call to action. Communities that coordinate better care, connect people earlier, and stabilize core needs will see fewer mental health crises. At Cloud 9, we’re proud to help our partners build that kind of future where care is collaborative, and prevention is possible.






